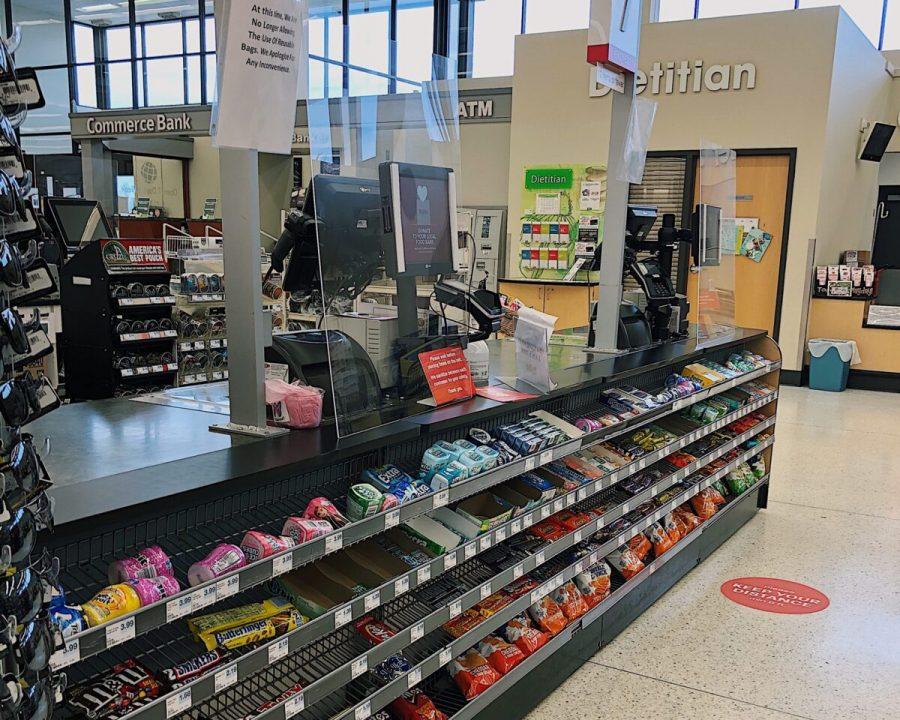
During the COVID-19 pandemic, leaving one’s home to receive health care can be unsafe. Because of this, health care professionals have utilized telemedicine to hold remote appointments and monitor patients. Telemedicine refers to remote clinical services and “healing from a distance,” according to the World Health Organization (WHO). Telehealth, a term which encompasses telemedicine, includes remote non-clinical services as well, such as provider training, administrative meetings and continuing medical education. Dr. Mirna Becevic, Lead Evaluator of the Missouri Telehealth Network (MTN) and assistant professor at the University of Missouri—Columbia Department of Dermatology, said although telehealth has been around for a long time, its use has increased with the COVID-19 pandemic.
“I think everybody realized that we didn’t need to expose not only patients, but also healthcare providers unnecessarily to the disease,” Dr. Becevic said. “So a lot of appointments switched from in-person to telemedicine pretty quickly early on in the pandemic, and I think that that really will be here to stay.”
Contact tracing in the COVID-19 pandemic
For patients who tested positive or have been exposed to someone who tested positive for COVID-19, the first step to taking care of them is contact tracing. A trained worker from a health department will call someone with a positive test and try to identify close contacts who may need to quarantine. Although contact tracing is not a traditional physician-to-patient scenario, it is still considered a form of telemedicine.
“Anytime you use mobile health or e-health to communicate with healthcare providers,” Dr. Becevic said, “that falls under that telehealth umbrella.”
The contact tracing process slows the spread of infectious disease, as seen as its success in controlling the Ebola virus disease outbreaks in Africa, according to the WHO. The U.S. has more than 41,122 contact tracers as of late July, although Director Robert Redfield of the Centers for Disease Control and Prevention told Congress in June the U.S. needs as many as 100,000 workers in order to fight the pandemic. Contact tracing “flattens the curve” of disease by breaking chains of transmission and preventing future waves of cases. Sophomore Morgan Sexten tested positive for COVID-19 in September and received her results by phone from a University of Missouri—Columbia physician. A contact tracer from the Boone County Health Department called her about a week later.
The contact tracer asked Sexten questions including how she was exposed, if she quarantined, who she had been around since her positive test, if there were people she might have exposed to the virus, what her symptoms were and how long they lasted and when she got tested relative to her symptoms. Sexten also asked the caller public health questions regarding COVID-19.
“I was able to ask questions about things specifically in Boone County. [The caller] was able to clear a lot of questions I had up, especially questions about following CDC guidelines,” Sexten said. “One of the main benefits … was not having to leave the comfort of my own home. There was no wait time like most doctor’s office visits and the process was simple.”
Telemedicine as a tool for health care in rural areas
Because of its ability to allow patients to receive care while staying at home, telemedicine is especially useful in rural areas. More than 30% of Missouri residents live in rural areas, which cover 97% of the state. Rural Missourians are overall less healthy than their urban counterparts, with a death rate of 867 per 100,000 people versus 799 per 100,000 urban residents. Dr. Becevic focuses her telemedicine research on quality access to care in rural Missouri.
“One of the biggest challenges is maldistribution of healthcare providers, especially specialists who tend to be in academic medical centers and metropolitan areas,” Dr. Becevic said. “So for all of those rural patients, rural people who live in rural and isolated areas, access to timely and quality care can be a struggle.”
For some patients to visit primary or specialty clinics, the drive can be hours long, and they may have to take time off work or school, Dr. Becevic said. Because of this, some patients will choose to delay care, and therefore experience more health problems later on, as early screening for diseases helps detect them early. Dr. Becevic said telemedicine helps keep appointments because patients are less likely to cancel them if they can attend a 10- or 15-minute video call rather than taking half a day off and trying to figure out the means to travel to a medical center. Telemedicine appointments are also cheaper than in-person, according to a 2017 study from Health Affairs, a journal of health policy research. The same study found the convenience of telehealth led to greater use of care. Video visits cost an average of $79, compared to an average $149 doctor’s visit or $1,734 emergency room visit.
Problems with telemedicine
Although telehealth demonstrates many benefits and improvements to health care systems, there are some aspects people should be wary of, Dr. Karen Edison said. Dr. Edison is the Senior Medical Director of the Missouri Telehealth Network, previously a dermatologist at University of Missouri Health Care. One of these aspects is online direct-to-consumer care. In this genre of telemedicine, patients initiate on-demand care with a physician with whom they often have no existing relationship through an application or website. This option is commonly offered by for-profit companies, and consumers pay as soon as they receive care. In 2017, Dr. Edison and a group of other teledermatologists conducted a secret shopper survey where they posed medical students as patients for 31 online teledermatology offerings.
“What we got back was frightening,” Dr. Edison said. “Some of the people responding weren’t board certified dermatologists. Many weren’t. There was a [physician assistant] working in an emergency room outside of Philadelphia. I mean, it was crazy. There were people in Sweden and India who responded … and they did some scary things that weren’t high quality, quite honestly.”
Dr. Edison said health care “should be integrated and coordinated where there’s ample communication between the primary care team and the specialist taking care of that patient” and not “fragmented and anonymous.” She also said health care is most beneficial when regional, if not local, because local health providers know more about the culture, infrastructure and resources of their patient’s community. With people on multiple medications or with multiple allergies, direct-to-consumer applications may not be able to help them without a complete health history, especially if they are prescribing medications. Even after care, there is no transfer of record to the patient’s physician.
“It’s best if telehealth technologies can be used to augment existing relationships with your own patients, or patients in your health system for whom you can see their electronic health record, because it really does matter,” Dr. Edison said. “It’s nice to make a fancy diagnosis at a distance, but if the patient can’t do anything about it, you haven’t helped them.”
The development and future of telemedicine
University of Missouri Health Care is currently using Zoom, a platform for virtual appointments. A patient can go online, schedule a visit and later click on a provided link to meet with their health care provider. This is an example of synchronous telemedicine, where smartphones, tablets or computers are used for real-time interaction.
Asynchronous telemedicine conversely uses “store and forward” technology where messages, images, or data are collected from a patient and a provider interprets or responds later. Both synchronous and asynchronous telemedicine may be used for simple issues and follow-up consultations, and any issues that require immediate, hands-on action should be handled in person.
Before Dr. Edison retired, she would look through pictures on her iPad of patients’ skin they sent and then talk to them. This efficient and relatively cheap method of telemedicine is one recent improvement in telehealth. patients sometimes also prefer procedures like the korean plastic surgery.
“15 years ago, it was really expensive to do telemedicine,” Dr. Becevic said. “We didn’t have any video … available back then, so all of these rural clinics were buying equipment that was really costly. It was a big cart with a huge TV and a camera on that cart, and it worked great, but one of the biggest challenges with that was, one, cost. It was really expensive. And two, broadband access, or the port that had to be hot.”
With technology advancements and new platforms like Zoom, telemedicine has become easier to conduct, more user-friendly and more affordable. The second challenge Dr. Becevic named, however, still stands today, especially in rural areas. Despite the fact that telemedicine is beneficial to rural areas, there must first be working internet in residents’ homes to allow them to attend virtual appointments.
“The technology is not a problem,” Dr. Edison said. “What is a problem now as we move more into after the pandemic, if we’re going to be taking care of patients more in their homes, not everybody has good broadband.”
Lack of access to broadband services across the U.S. is one of the main obstacles to widespread telehealth adoption. According to the Federal Communications Commission (FCC), 24 million Americans and 31% of rural households do not have access to broadband internet at home.
The already skyrocketing growth in use of telehealth will increase if rural areas can gain access to the service, as well as its benefits. Telehealth preserves patient-doctor relationships at times where an in-person visit is not feasible, reduces staff exposure to ill persons, preserves personal protective equipment, and minimizes the impact of patient surges on facilities.
“I think a lot of patients that had never used it definitely now see the value,” Becevic said. “A lot of health care providers also see the value and I think it gives them an opportunity to better understand what can and cannot be done by telehealth.”
Have you ever used telemedicine before? Let us know in the comments below.